The Cost of Capitalism?
For-profit Healthcare
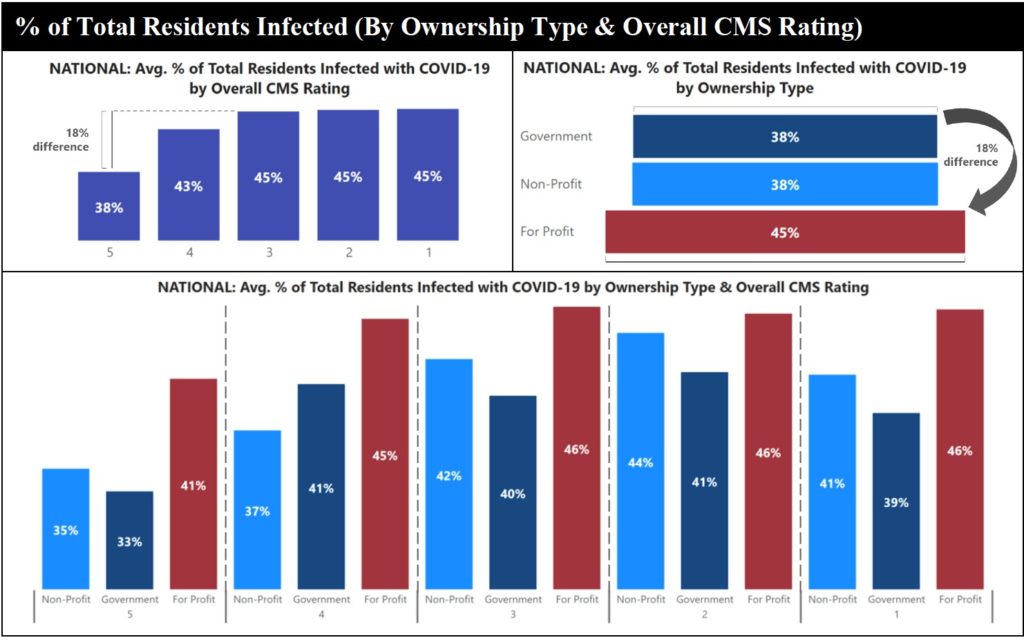
People always complain about universal health care as socialism. They assume a not for profit health care system would negatively affect the quality of care. However, that does not appear to be true. For example, federal data shows that for-profit facilities were 18% less effective with preventing COVID-19 infections than nonprofit or government-run facilities.
The Center for Medicare Advocacy blasted staffing shortages, unsafe infection control standards, systemic problems, and mismanagement caused the unsafe conditions. A new report called “Geography Is Not Destiny: Protecting Nursing Home Residents from the Next Pandemic” calls on more enforcement. Geography was less a factor in spread than ownership type or staffing.
Using the CMS’ COVID-19 dataset and its Care Compare database, the advocacy compared COVID infections with ownership, star ratings, and staffing level variables.
“For-profits were the worst performers across every CMS rating pool,” author Cinnamon St. John said.
Solutions
U.S. billionaires added more than $1 trillion to their wealth in 2020. However, the U.S. suffered the sharpest rise in poverty rate in 50 years. By January 2021, the combined fortune of the 660 billionaires in the U.S. had exceeded $4.1 trillion, an increase of more than 38% since the beginning of the pandemic. The fortunes of the wealthiest 15 billionaires increased more than 58%.
This is not new. It was also true before COVID. The GAO found investigators most often cited infection prevention and control deficiencies in nursing homes between 2013 and 2017. Some 82% of facilities had an infection violation, and 48% cited in multiple years. Yet regulators only sanctioned 1% of the deficient homes.
“The problems in infection control were treated as not serious,” said Senior Policy Attorney Toby Edelman. “We know now how wrong that was.”
St. John proposed a series of solutions including increasing RN staffing, improving wages and benefits for direct care staff, and lowering the number of residents per room. In addition, the industry needs a full-time infection preventionists in every facility.
The key is safe staffing with competent and qualified caregivers working within their scope of practice and education.

Recent Comments