Patient-Driven Payment Model
Data on PDPM
Skilled Nursing News had a great article explaining how the Patient-Driven Payment Model (PDPM) is a windfall to nursing homes. The PDPM is the reimbursement change to Medicare for skilled nursing facilities. It took effect in October of 2019 so we have one year of data. However, this has not been a typical year.
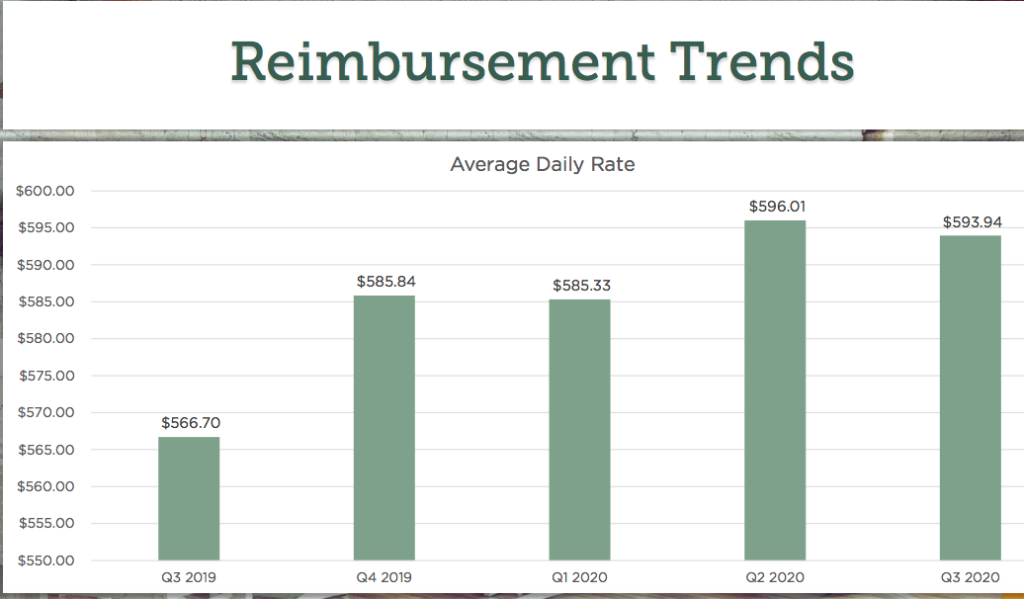
The data shows that PDPM has been costly. It has not been revenue-neutral as promised. The new system was designed to have government spending stay the same as it had been under the old Medicare reimbursement model, the Resource Utilization Group (RUG) system. But the average daily rate generally rose from the third quarter of 2019 until now.
Manipulating Assessments
The reason for that lies in the self-reported assessments in the Minimum Data Set (MDS). Under PDPM, providers are reimbursed based on what the nurse determines the levels of care a resident needs to maintain the health, safety, and well-being of the resident. The five key areas: physical therapy (PT), occupational therapy (OT), speech therapy (ST), nursing care, and non-therapy ancillary services.
“Across the country, we saw daily rates increase under PDPM,” an expert explained. “The reason it was not revenue-neutral was because CMS had planned for MDS coding to remain the same. So they set the case mixes at exactly the right amount, so that total rates would not change. They never counted on people changing the way that they coded post-PDPM.”
The nursing home can manipulate the assessment to get more reimbursement with less care. For example, depression remains a critical one; before PDPM, less than 1% of residents were positive for this condition, but now it’s about 8%. Another is whether or not a patient qualifies as “special care high” has seen a significant increase. This adds $45 a day in the nursing payment area.
Another critical area for operators is that of quality measures. The physical and emotional toll COVID-19 has taken on residents and families is still coming into focus. While falls with injury have dropped 17% from the 2019 fourth quarter compared with the three months ending July 31 of this year, several other problems have emerged. Loss of movement is up 55%, loss of activities of daily living is up 15%, and unexplained weight loss is up a troubling 65%, according to TMC.
However, nursing home operators will have to cut the amount of therapy services they can offer, thanks to Trump’s Medicare payment cuts. A 9% cut to payments for physical and occupational therapy was included in the Proposed Physician Fee Schedule Rule for 2021 announced by the Centers for Medicare & Medicaid Services in early August. The therapy providers took an 8% cut last year.

Recent Comments